Bioengineer
19h
344
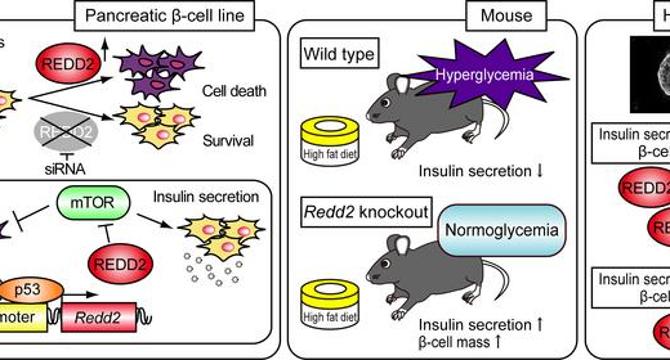
Image Credit: Bioengineer
Stress-Activated Gene Linked to Diabetes Uncovered in New Study
- Researchers at Osaka Metropolitan University discovered a gene, REDD2, exacerbating pancreatic β-cell dysfunction under metabolic stress, shedding new light on type 2 diabetes.
- REDD2's heightened activity under oxidative stress negatively impacts pancreatic β-cell function, marked by reduced insulin production and increased cell death.
- Overexpression of REDD2 inhibits mTORC1 signaling, critical for cell growth and survival, leading to impaired glucose tolerance and β-cell apoptosis.
- Studies show that suppressing REDD2 expression enhances β-cell survival and insulin secretion, offering potential therapeutic strategies for diabetes management.
- Human pancreatic islet cell analyses support REDD2's detrimental role in β-cell function, highlighting its relevance to human health and diabetes progression.
- Oxidative stress, driven by lifestyle factors like overnutrition, activates REDD2, linking metabolic signals to β-cell damage and diabetes development.
- Identifying REDD2 as a biomarker holds promise for early detection of β-cell stress and the development of interventions to preserve pancreatic function and prevent diabetes onset.
- The study underscores the complex interplay between genetic, metabolic, and environmental factors in the progression of type 2 diabetes, offering insights for future research and therapeutic approaches.
- The research highlights REDD2 as a potential therapeutic target and biomarker for β-cell vulnerability, aiming to address the root causes of diabetes beyond symptomatic treatments.
- The findings emphasize the significant impact of REDD2 in linking metabolic stress to cellular dysfunction in pancreatic β-cells, paving the way for innovative diagnostic and therapeutic avenues.
Read Full Article
20 Likes
For uninterrupted reading, download the app